The History and Types of Bariatric Surgery
History of Bariatric Surgery Classification
Historically, weight loss surgeries were classified based on their supposed mechanisms of action. Adjustable gastric banding was considered as a purely restrictive surgery, but a high long-term complication rate associated with weight regain, slippage and erosions has led to a loss of interest in this procedure in favor of surgeries with a metabolic impact. Hypoabsorptive surgeries were thought to decrease the absorption of nutrients by bypassing portions of the small intestine (i.e., gastric bypass or duodenal switch). However, mechanistic studies have described many metabolic modifications, including changes in incretins, gut hormones, bile acids levels, and microbiota, which has led to referring to these surgeries as “metabolic operations.”
What Bariatric Surgery is Right for Me?
The decision for the type of surgery is made by your bariatric surgeon based on the patient’s medical condition, including weight, obesity-related diseases, expected adherence with supplementation and follow-up, patients’ personal goals and preferences in terms of expected weight loss, resolution of comorbidities, and side effects.
The goal is to find a balance between the complications and risk of mortality associated with obesity itself, to improve the patient’s quality of life (QOL), and reduce obesity-related diseases while aiming for acceptable short- and long-term complications and side effects related to the surgery itself. As a rule of thumb, early and long-term risks and side effects, but also maintenance of weight loss and remission of comorbidities, are proportional to the intestinal bypass. Other bariatric procedures such as single-anastomosis duodeno-ileostomy and single-anastomosis gastric bypass are becoming more popular, but are still lacking substantial scientific rationale.
Adjustable gastric banding
Adjustable gastric banding is one of the procedures that has evolved the most over the last 20 years, from a non-adjustable gastric band performed by laparotomy to laparoscopically performed adjustable gastric banding. Iterations of the technique have always aimed to reduce the complications that appeared over time. The procedure consists in placing an adjustable silicone band at the level of the cardia, creating a small stomach pouch above the band, with the rest of the stomach below the band. The gastric band is connected by a silicone tube to a subcutaneous reservoir. The reservoir can be inflated or deflated to control the opening between the pouch and the remainder of the stomach. Even though this procedure is associated with the lowest short-term complication rate, it is associated with a high long-term complication rate and weight regain, which has led to its progressive replacement by sleeve gastrectomy.
Sleeve gastrectomy
Sleeve gastrectomy was first used by laparoscopy as a staged approach in order to reduce peri-operative complications in high-risk patients. Interestingly, some patients experienced appreciable weight loss with the sleeve gastrectomy alone and did not require second-stage surgery, thus avoiding the side effects of malabsorption. Its relative technical simplicity and good outcomes led to a worldwide surge in popularity as a stand-alone procedure, starting around 2008. This procedure involves resection of the lateral part of the stomach to create a narrow gastric tube along the lesser curvature. It promotes weight loss through reduced meal volume and reduced appetite. It has become the most frequently performed surgical approach, representing 45.9% and 58.3% of all surgeries in the world and in North America. In addition, sleeve gastrectomy is typically easier to revise in case of weight regain compared with Roux-en-Y gastric bypass.
Roux-en-Y gastric bypass
Roux-en-Y gastric bypass involves the creation of a small gastric pouch at the level of the cardia. This pouch is connected to the proximal small bowel by bypassing the first 75–150 cm and bringing a 100–150 cm alimentary limb onto the gastric pouch. Short-term metabolic and hormonal effects have been studied extensively in numerous studies.24 It has been considered as the gold standard in bariatric surgery until recently when it was supplanted by sleeve gastrectomy.
Duodenal switch
The duodenal switch combines moderate restrictive and hypoabsorptive mechanisms by creating a wider sleeve gastrectomy, while the duodenum is transected distal to the pylorus and anastomosed to a 250 cm alimentary limb, leaving a 100-cm common channel for nutrient absorption. Duodenal switch reduces morbidity and mortality, improves T2DM, and corrects many features of the metabolic syndrome in long-term studies. This operation compares very advantageously with the other surgical options available, offering the most pronounced and durable weight loss and 80–90% remission rates .
Yet, the technical complexity and the risk of long-term nutritional deficiencies have hindered its widespread use. According to the most recent data, duodenal switch represented 1.1% of the total number of surgeries worldwide.
Next Steps
If you are considering bariatric surgery and would like to arrange a teleconsultation, or request a quote we would be pleased to support you with this and help you on your path to health and wellness. You can also review bariatric price guides here.
Remote Patient Monitoring (RPM): How Taqtik Health Helps Patients and Providers Stay Connected
Remote Patient Monitoring (RPM) is changing how healthcare providers support patients between visits. By using secure digital tools, RPM allows care teams to monitor patient progress remotely, improve engagement, and reduce administrative workload. Taqtik Health offers a modern Remote Patient Monitoring platform designed to support healthcare programs with simple onboarding, clear progress tracking, and secure...Continue reading→
Taqtik Health RPM: Your Partner in Post-Bariatric Surgery Success
At Taqtik Health, we understand that bariatric surgery is a powerful step toward a healthier, more fulfilling life. But we also know that the journey doesn’t end in the operating room. The real challenge and the real transformation happens in the months and years after your procedure. That’s why we created Taqtik Health Remote Patient...Continue reading→
Post-Bariatric and GLP-1 Post-Care to Maximize Results
Post-Bariatric and GLP-1 Post-Care to Maximize Results | Taqtik Health Introduction Undergoing bariatric surgery or starting GLP-1 (glucagon-like peptide-1) agonist treatments like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) is a major step toward long-term weight loss and improved metabolic health. But these treatments are only part of the journey. What you do after surgery...Continue reading→
Remote Patient Monitoring for Obesity: A Smarter Way to Support Surgical and Non-Surgical Patients
Losing weight and improving your health is a personal journey—and it doesn’t always require surgery. Whether you're preparing for bariatric surgery, recovering from it, or trying to manage your weight and health without surgery, one thing remains constant: support matters. At Taqtik Health, we believe long-term success comes from daily progress, consistent accountability, and expert...Continue reading→
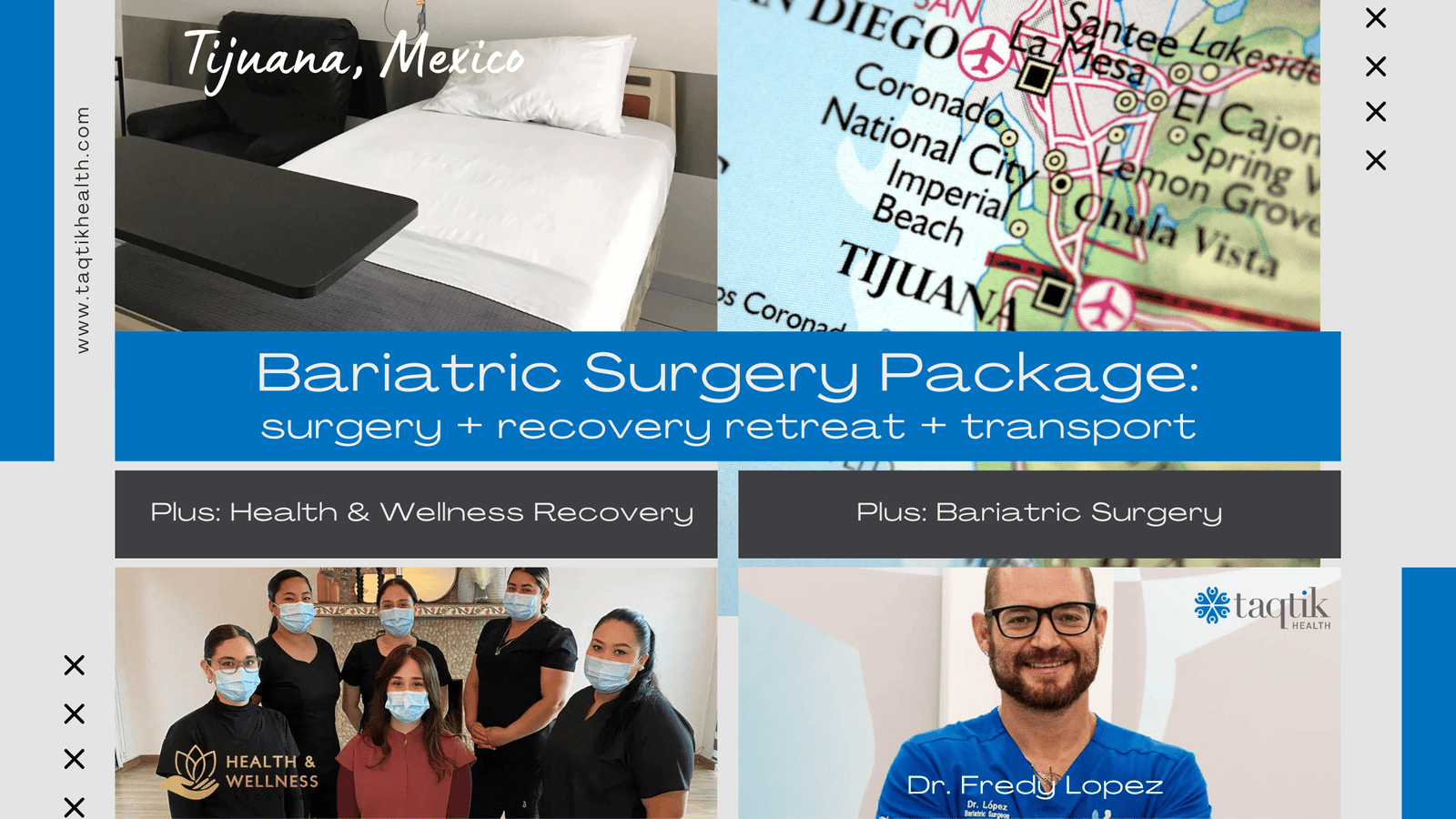
Bariatric Center J.L. Prado in Tijuana, Mexico: Your Destination for Advanced Weight Loss Surgery
Bariatric surgery has become a life-changing solution for individuals struggling with obesity and its related health complications. In recent years, Tijuana, Mexico, has emerged as a leading destination for affordable and high-quality bariatric procedures. One of the most trusted names in this field is Bariatric Center J.L. Prado, where a team of skilled surgeons, cutting-edge...Continue reading→
Transform Your Life with Our Bariatric Surgery Promotion in Tijuana Mexico
Transform Your Life with Bariatric Surgery at J.L. Prado Surgical Center in Tijuana, Mexico, with Dr. Fredy Lopez Are you ready to take control of your health and achieve long-term weight loss? Taqtik Health is excited to offer a special promotion for bariatric surgery at J.L. Prado Surgical Center with the renowned Dr. Fredy Lopez,...Continue reading→
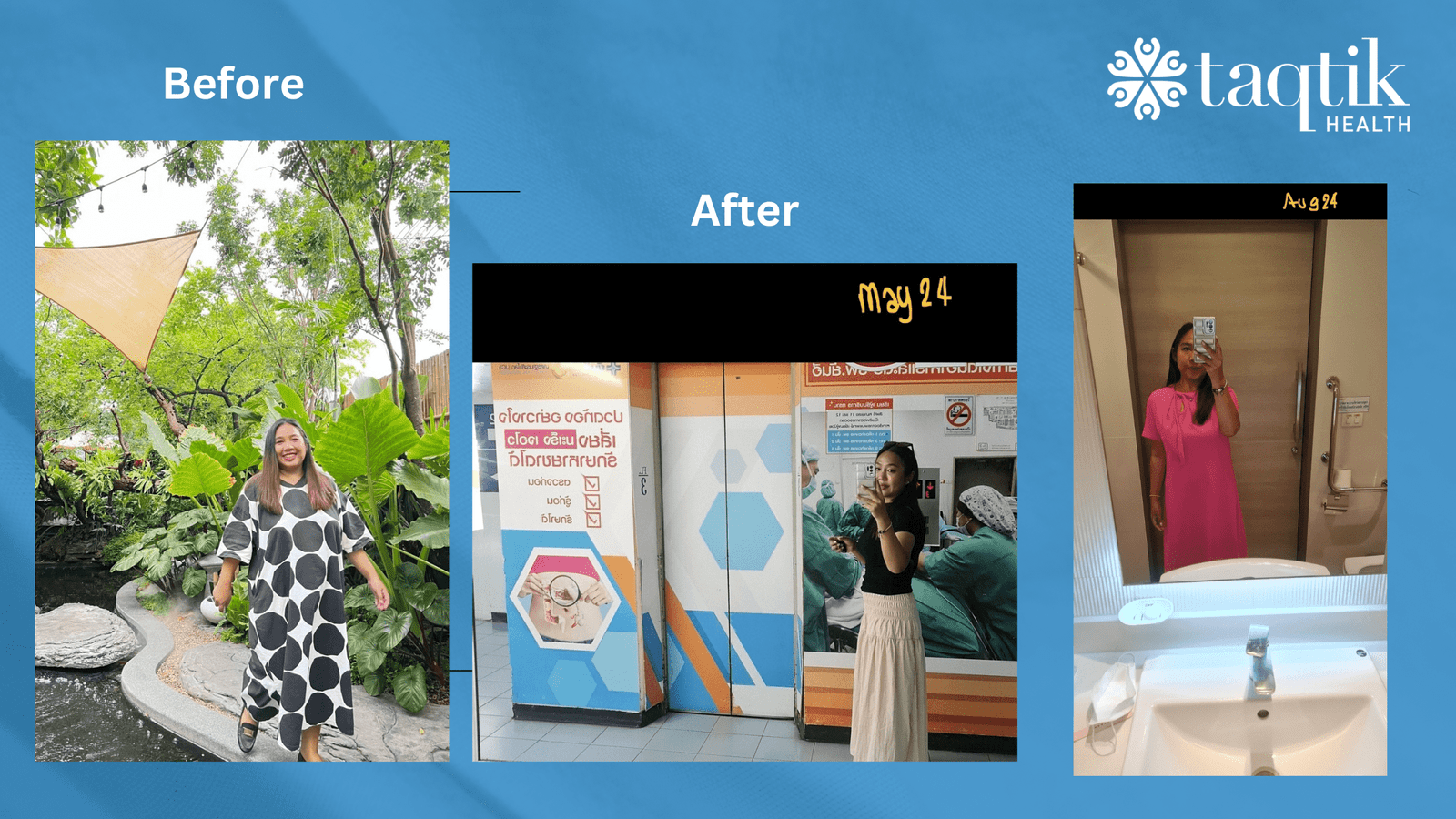
Bariatric Surgery Case Study: Kael Sangnam
Background: Kael Sangnam, a 37-year-old with a BMI of 34.7, had been struggling with several health issues, including sleep apnea, shortness of breath, and persistent back pain. Despite various attempts to manage her weight, these health conditions continued to affect her quality of life. Realizing that these conditions were closely linked to her weight, Kael...Continue reading→
How to Choose the Right Bariatric Procedure or Weight Loss Solution
Choosing the right weight loss solution is a deeply personal decision that depends on various factors, including your health, lifestyle, and goals. At Taqtik Health, we understand the complexities involved in making this choice and aim to provide you with comprehensive information to help you make an informed decision. This guide will explore the different...Continue reading→
Transformative Journeys with Taqtik Health: Sarah and Miguel’s Stories of Bariatric Surgery and Total Body Makeover
Introduction The decision to transform one's body and regain health is a profound and personal journey. For many individuals, bariatric surgery is a crucial first step towards achieving a healthier lifestyle. However, the journey doesn't end there. In this blog, we share the inspiring stories of Sarah and Miguel, who chose Taqtik Health to assist...Continue reading→
How to Choose Your Ideal Destination for Bariatric Surgery: Cost Considerations and Factors
Welcome to Taqtik Health, where we pride ourselves on helping you make well-informed healthcare decisions. Bariatric surgery is a life-changing procedure, and choosing the right destination for your surgery is crucial for a multitude of reasons. To make your decision easier, we've put together this comprehensive guide featuring top medical tourism destinations for bariatric surgery:...Continue reading→